-
Topics
subnavigation
Topics
Electromagnetic fields
- What are electromagnetic fields?
- Static and low-frequency fields
- Radiation protection relating to the expansion of the national grid
- High-frequency fields
- Radiation protection in mobile communication
Optical radiation
Ionising radiation
- What is ionising radiation?
- Radioactivity in the environment
- Applications in medicine
- Applications in daily life and in technology
- Effects
- What are the effects of radiation?
- Effects of selected radioactive materials
- Consequences of a radiation accident
- Cancer and leukaemia
- Genetic radiation effects
- Individual radiosensitivity
- Epidemiology of radiation-induced diseases
- Ionising radiation: positive effects?
- Risk estimation and assessment
- Radiation protection
- Nuclear accident management
- Service offers
-
The BfS
subnavigation
The BfS
- About us
- Science and research
- Laws and regulations
- BfS Topics in the Bundestag
- Links
Diagnostic nuclear medicine
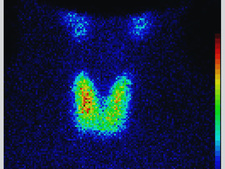
![]() Thyroid gland scintigraphy
Source: Technical University of Munich, Clinic and Policlinic of Nuclear Medicine, Klinikum rechts der Isar
Thyroid gland scintigraphy
Source: Technical University of Munich, Clinic and Policlinic of Nuclear Medicine, Klinikum rechts der Isar
Patients in diagnostic nuclear medicine are given radioactive pharmaceuticals (radiopharmaceuticals) accumulating in organs and tissues in varying concentrations, depending on the pharmacological properties of the compound administered. Due to their radioactivity, the spatial and time distribution of the radiopharmaceutical in the body is detectable using proper measuring equipment, and thus can be visualised.
Which technology is used?
Basically there are three different technologies:
- conventional scintigraphy
two tomography procedures:
- positron emission tomography (PET)
- single photon emission computerized tomography (SPECT).
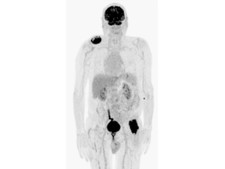
![]() Malignant melanoma of the forehead; Two soft tissue metastases right shoulder / left hip.
Source: Technical University of Munich, Clinic and Policlinic of Nuclear Medicine, Klinikum rechts der Isar
Malignant melanoma of the forehead; Two soft tissue metastases right shoulder / left hip.
Source: Technical University of Munich, Clinic and Policlinic of Nuclear Medicine, Klinikum rechts der Isar
When are diagnostic nuclear medicine procedures applied?
Diagnostic nuclear medicine enables almost all organ systems of man to be examined. It provides information on the function of organ systems in question as to both general dysfunctions (for example renal function scintigraphy) and localised foci in individual organs (for example, detection of foci of inflammation). Diagnostic nuclear medicine is a valuable extension of so-called morphologic imaging procedures used to visualise the form and structure of organs or tissues under examination (for example, X-ray diagnostics).
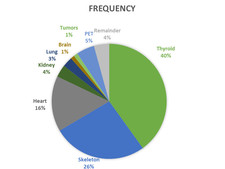
![]() Relative contribution of different examination types to total frequency in 2014
Relative contribution of different examination types to total frequency in 2014
How often are diagnostic nuclear medicine procedures applied?
The annual mean number of nuclear medicine examinations carried out in Germany between 2010 and 2014 was about 3 million, corresponding to a mean annual frequency of applications of about 34 examinations per 1,000 inhabitants. Thyroid and skeleton scintigraphy were the most frequent examinations. The mean annual effective dose per inhabitant and year was about 0.1 millisievert (mSv).
Three procedures predominate
The following three procedures contribute most to the total frequency of nuclear medicine examinations as well as to the associated collective effective dose, that is, scintigraphy of
- the thyroid gland,
- the skeleton, and
- the heart (see figure above).
Note that in the figure, scintigraphies of the heart during rest and during exercise are counted separately, even if they are performed in the course of one examination (during one day or two consecutive days).
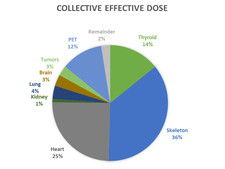
![]() Relative contribution of different examination types to total collective effective dose in 2014
Relative contribution of different examination types to total collective effective dose in 2014
Mean effective dose per procedure
Averaged over all examinations carried out, the mean effective dose per procedure is 2.4 mSv. Thyroid scintigraphy is most frequently used and is associated with a quite low mean effective dose of 0.9 mSv per examination. Renal examinations are relatively frequently applied in children, and are also characterized by low radiation exposure (0.7 mSv per examination). Adding the doses for scintigraphies of the heart during rest and during exercise, the resulting dose is relatively high: ca. 8 mSv per examination.
Comparison with radiation exposure from diagnostic radiology
Nuclear medicine examinations are considerably less frequent than X-ray examinations. The mean effective dose per caput from diagnostic nuclear medicine, therefore, is relatively low compared with the mean per caput effective dose from diagnostic X-rays amounting to 1.6 mSv per inhabitant in 2014.
State of 2018.03.01


